This was originally published on http://www.almostdocs.com (which doesn’t exist anymore???) in May 2014. Jean passed away in September 2016. I am sharing this again here in her memory.
I first had the pleasure of meeting Jean Smelker nearly a year ago. I had just finished undergrad and was on my way to start medical school and graduate school in the fall. Jean, a retired pediatrician with a soft voice and a beaming smile, was so excited to hear about my journey (though I’m sure I was more excited to hear about her’s.)
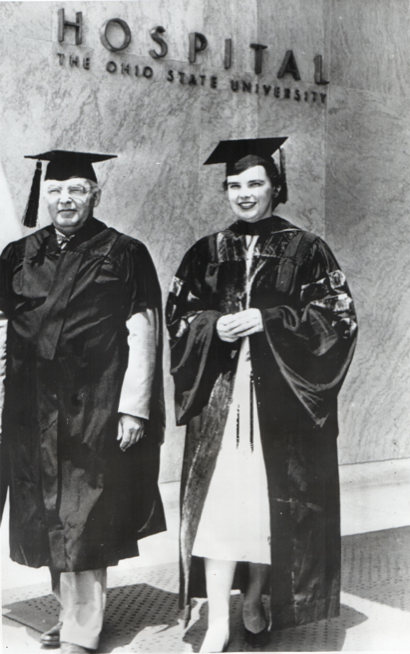
You see, Jean went to medical school in the early 1950’s, a time when women physicians were rare. In fact, she was the sole woman in her medical school class of 75. In addition to her training as a MD, she earned a master’s degree in immunology and a master’s degree in public health, which came in handy as she served as director of two Children and Youth (C&Y) Projects throughout her career (one in Kansas, the other Minnesota) that provided comprehensive health services for children living in low incomes areas.
She proved to be very bright and ahead of her time, becoming known as a progressive and holistic physician. Her philosophy that “We do what is best for the patients and make it work” became a guiding principle for the Minnesota C&Y project, and she was renowned for her use of hypnosis to treat warts.
On top of her serving as director of these projects and later commuting between Minnesota and Ohio for work, she managed to raise her children with her psychiatrist husband Ed who pioneered the study and care of patients with PTSD. Of course, being able to balance successful careers with raising children such as they did is an amazing feat in itself!
Jean is a personal inspiration and role model, and so it is my honor to share some of her story here on The Almost Doctor’s Channel with hopes that she will inspire many other almost docs as well.
Hanna Erickson: First of all, how did you decide to do medicine? Did you have any specific role models in medicine that you looked up to? How did you prepare yourself for medical school and what was the application process like?
Jean Smelker: I started out in Occupational Therapy. I was 16, it was the end of WWII. It was interesting, but the courses didn’t go very deep – just when they got interesting, we started on something else. I thought I wanted something “more scientific.” I switched to Bacteriology at the end of my Freshman Year. It was certainly interesting, with a lot of changes because of WWII. Things were happening very fast, new developments. In my senior year I decided to go on to Immunology for my M.Sc., where changes were even faster. I loved it, but I wasn’t sure I was cut out to do pure research. Every time we did an experiment, I could think of half a dozen ways to proceed – but one team member (on a PhD track) could think of a dozen ways to go. (He was very smart.) And, I was not certain I wanted to work with the same half a dozen people, behind a test tube, the rest of my life.
Then, one day, my Dad came home from a meeting with some of his Faculty buddies. Dr. Ralph Knouf of Comparative Anatomy said, “If Jean ever needs a referral to Medical School, I would gladly give her one” and I thought and thought about it. (That was December, I had just finished the Comparative Anatomy course.) Did I want an M.D. rather than a Ph.D? I applied, and got my acceptance on Valentines Day. (To which my Mother said, “Well, I guess that’s the kind of Valentines you’ll be getting from now on.” Was her idea of going to college to get a “Mrs.”? Probably. My younger sister was about to be married – and I was on the way to being an ‘old maid’ I guess.) This sounds sort of haphazard today, but there really was a lot of thinking going on about the decision.
No, I didn’t have any role models. There was one woman physician who had died recently. I remember she had a pretty winter coat (this was Ohio) but I really didn’t know anything about her! My childhood pediatrician came closer to being a role model, Dr. Earl Baxter. His daughter was a couple of years ahead of me in University School. (Ohio State.) I am sure that being a faculty kid and being in the University milieu was more influential, really. Interviews in those days were quite a lot different too, of course. I remember being asked – in a very persistent way, “If your own kid was very ill and one of your patients (kid) was very ill, what would you do? ” That kind of question wouldn’t cut it today, thank goodness. (I think I later lived the answer to that question, more than once.)
So, I had a B.Sc. and a M.Sc., going into Medical School. I was a lab assistant for the Medical Bacteriology class – where I met my husband to be. And I had taken the Medical/Dental Chemistry sequence at University of Michigan one summer, as part of my M.Sc. So, I had a sort of head start, that first year.
HE: What was medical school like? How did being female alter your experience? Do you feel that your teachers and/or your peers treated you differently than your male counterparts?
JS: In 1950 there were still a lot of ex G.I.’s coming into Medical School. I was the only woman in my class of 75. The class next to me had 3 women – Eileen Ferrell, Catherine Panis and LeMoyne Unkefer. The only time I can remember when it made a significant difference was the day we had two choices in a lab course – gastric analysis and the 3-hour urinary glucose tolerance test. I had to do the quite uncomfortable gastric analysis – because there were NO Women’s Bathrooms in the ENTIRE Kinsman Hall!
The rest of the time, I think one had to ignore the male/female thing. I know there were things, but being the only one, it didn’t pay to notice. I was lucky because my husband’s medical fraternity brothers accepted me, so I could study with them and they looked out for me. It was the lab assistants, etc., who were more likely to try to sneak in a pinch or two. And, I think I liked it the way it was – not much change because of my sex. I had gotten accustomed to that in Grad School, I think.
HE: What was your favorite part of medical school? Your least favorite part?
JS: I think a defining part of Medical School was the “Physical Diagnosis” course in the Spring Quarter of Sophomore Year. I had often felt really privileged to be taking the Medical School courses as I went along, but this course taught subtle things that doctors are taught that make you a doctor for the rest of your life. It separated me from all my long time “girl” friends. It was the real beginning of what made me an M.D. instead of a Ph.D. And, I didn’t realize it until some time afterwards.
I just liked the whole experience, exciting new material all of the time. I remember our Dermatology instructor especially. He was really good. He had a lot of slides and his descriptions were top notch. By the end of each class, if you looked around the room, everybody was scratching! The worst was our Physiology instructor. He was German with a VERY strong accent. For the whole first week we thought he was saying, “squirrel muscle” instead of skeletal muscle. That was his specialty and the course lacked depth. When we got to Boards, thank goodness I had the Physiol. Chemistry from University of Michigan to fall back on.
I really didn’t have many ‘unfavorite’ parts, as I said – it all seemed such a treat that so many others didn’t enjoy. I hated being on call more during internship (in a pre-Vatican Roman Catholic Hospital) after I got pregnant as a sort of ‘punishment’ – even though I had done extra covering for a couple fellow interns who got ill. (I was so fortunate in having classmates who always treated me fairly.)
HE: How did you keep yourself going throughout medical school?
JS: As I look back, I think one of the things that kept me going was observing my husband, who was two years ahead of me. He was always an important role model, although our specialty choices and much else, was very different. But it helped me move ahead, having some idea of what was coming.
HE: How did you decide on your specialty?
JS: Deciding on a specialty was a subtle thing. It wasn’t until some years later that I really figured out what was going on. I was the oldest of 4 girls – and from an early age, ‘responsible’ for us all, in a way. My sister 2 years younger (a tennis champion and very independent) who was not a ‘follower’ took some extra skill. The third sister was a sweety. A month after her 8th birthday and a month before my 14th birthday, she died suddenly of typhoid fever. (Her friend lived in the country and there was a little stream they often played in – this was 1943.) It was a huge thing for the family, of course, but it wasn’t until a number of years later that I realized the role that played in my choosing Pediatrics.
Other circumstances played a part, of course. It was easier for women to get into at the time, of course. The Family Practice residences were just gearing up, but I didn’t see how I could possibly learn everything for every age group that that would require. Also, with my husband specializing in Psychiatry, city life seemed ordained and the Family Practice residencies had a lot of rural tilt. (If it had been 30 years later, I think I would have opted for some time in third world countries.)
HE: What was your career like? Where did you work?
JS: Choosing the inner city Federal “Children and Youth Projects” was a perfect fit, after some years in private practice. I was the “Clinical” Director of the C&Y project in Topeka, Kansas, which went to the Health Department and then the Director of the University of Minnesota sub-project of the Minneapolis Health Departments C & Y Project – the only Director of two different C&Y’s!
When we first moved to Topeka, KS we planned to stay for just a year. I did some Child Health Conferences for the Health Department that summer and then ‘covered’ for a “GP” who had a rural practice about 12 miles west of Topeka. That was a riot. The local Grange had built an office with a waiting room, two exam rooms, – a pump in one of the rooms- and an ‘outhouse.’ I went two mornings a week and an evening, to keep the practice running for him. It was a fantastic chance to follow several generations and do research in familial diseases.
When it became apparent that we would stay more than a year, Ed went on the Menninger Foundations faculty and I joined a Pediatrician in Topeka who was waiting for a long term partner. One of the difficult things for me was that the permanent partner arrived just as my daughter was born – and I had to decide – did I want to go into practice by myself, or what?
I did, we stayed in Topeka 15 years instead of one and I had the chance to head up the C&Y Project for nearly 3 years, until we moved to Minneapolis. My husband had the choice of moving to New Hampshire, Washington D.C. or Minnesota. Our children were just starting High School and Junior High School. We thought it might be tough for me to get a spot in small town New Hampshire and Washington might be okay – for awhile. We both had an easy time picking Minnesota. We moved in 1970, both into spots that we loved.
In time, the C&Y Federal Projects went local. We were able to improve Maternal and Child Health statistics for American Indian children and youth in our catchment area, to start not only Family Planning services, but also OB services, with the same results. Finally we were able – in 1976 – to start a program for all ages with the help of the University of Minnesota. This comprehensive program still exists.
In the mid 1980s, the Pediatrics Department in Minneapolis was in a muddle, with no Department head, and a friend had been forced to retire. I didn’t want the same sort of possibilities to happen to me. I had been very ill with Trigeminal Neuralgia and taken a 6 weeks sabbatical. (My first, ever.) I was well again on a great new medication (Neurontin) but the new Vice President for Health Sciences offered me a job doing clinical work only at the Community University Health Care Center for the following year.
I had been the Director of the Center from the summer of 1970 until I became ill in the fall of 1984, and I had my M.P.H. in Health Management and Health Policy from the University of Michigan, so I told this new VP ‘thank you, but no thank you.’ I did not think such a position was workable in a situation where I had been “boss” for so long. I negotiated a full year of salary and another year of half salary with Health Sciences so that I could work with Dr. Olness’ group in Minneapolis. This was, perhaps, the most draining period of my entire career and I probably could have parlayed it for more than I did. On the other hand, the work with Dr. Olness’ group was by far, the most creative.
My last 5 years was spent commuting from Cleveland, Ohio to our home in Minneapolis, MN. I was on the faculty at Case Western University and flew home 2 or so times a month. I had learned Brain Wave biofeedback and other forms of biofeedback when we lived in Topeka, Kansas – (at the Menninger Foundation.) Dr. Karen Olness was the Chief of our Service and we did many interesting things at Rainbow Babies and Childrens Hospital.
The stint at Case, in Cleveland, was really great. I had a lovely 1850 “workers Cottage” in Ohio City (Cleveland) and had time to make a beautiful garden. I ‘commuted’ home by air, 1-3 times a month. It was a good thing for a woman of my generation to manage a home by myself, as I had gone from my father’s house to my husband’s. It was perfect and I learned a lot. I worked at Case, in Cleveland, from July 1987 until July 1992 (or 93??) I retired a little early because my leg injury from age 12 was becoming a problem. (Surgery in 1948 lacked a lot – wish I had today’s improvements.)
HE: How did you balance work and raising a family?
JS: Getting good help is key. I can’t remember this being really a problem. I had a husband who always did his share without being reminded and kids who were alert, interested and creative. Certainly, getting good help cut into my income, but I always felt I had plenty, anyway. I was doing interesting work, I was doing useful work – what more could one want?
HE: If you had to do it again, would you still choose to do medicine? If so, would you pick the same specialty?
JS: First, I would always lean towards those most in need. And my M.P.H. in Health Management/Health Policy (Univ. of Michigan) would play a part as would my early training in Self Regulation at the Menningeer School in Topeka, Kansas. I would like to pick a catchment area where we could go in, with a team that could change the maternal and child health statistics in that area for the better. This team would include a Masters level Nutritionist, a Masters level Health Educator, Community Health Workers, a PhD psychologist, Pediatric and OB people, probably including Nurse Practitioners, and other folks necessary to run a clinical operation. Also, the capacity for Dental services.
I would use the model of the Federal Children and Youth Projects, where I was able to direct two of the 58 Projects. These Projects had a vision of health care delivery that has not been surpassed. The maternal and child health statistics would show improvement and the cost would be well below the going rate.
I would love doing some of the usual, regular routine of Pediatric Care – checkups were never a bore with children, the challenge of illness in the usual population – and enough time for administration to keep the vision going. Along with administration and routine pediatric care, I would like to have a defined piece of care time to do Brain Wave Biofeedback with a referral population. (I would do other pieces of self regulation within the regular pediatric care.) So, yes – the same specialty, brought very much up to date.
HE: What advice do you have for the new generation of physicians?
JS: Enjoy learning – it will lead you.
If you like my writing, please consider following my blog. There’s a link near the top of the side bar to do so. Also, feel free to like my Facebook page (MD, PhD To Be), follow me on Twitter (@MDPhDToBe), and follow me on Instagram (MDPhDToBe). I am trying my best to remain active in each of these channels throughout my training! Any questions, comments, or requests for future blog posts can of course be directed to me from any of these locations or directly emailed to me at via the connect page. Thank you for reading!